Clinical blood cell transfusion trial made safer
After Public Citizen raised concerns about ethical violations in a clinical trial involving heart attack patients, government agencies made changes.
- 3,500 Number of hospitalized adult patients who are to be enrolled in the trial.
- 10 Months it took the federal government to respond to Public Citizen’s complaint.
- 30 Days subjects would be studied to see if they die or have another heart attack.
In August 2017, Public Citizen called for an immediate suspension of the Myocardial Ischemia and Transfusion (MINT) trial over concerns about potentially serious ethical violations.
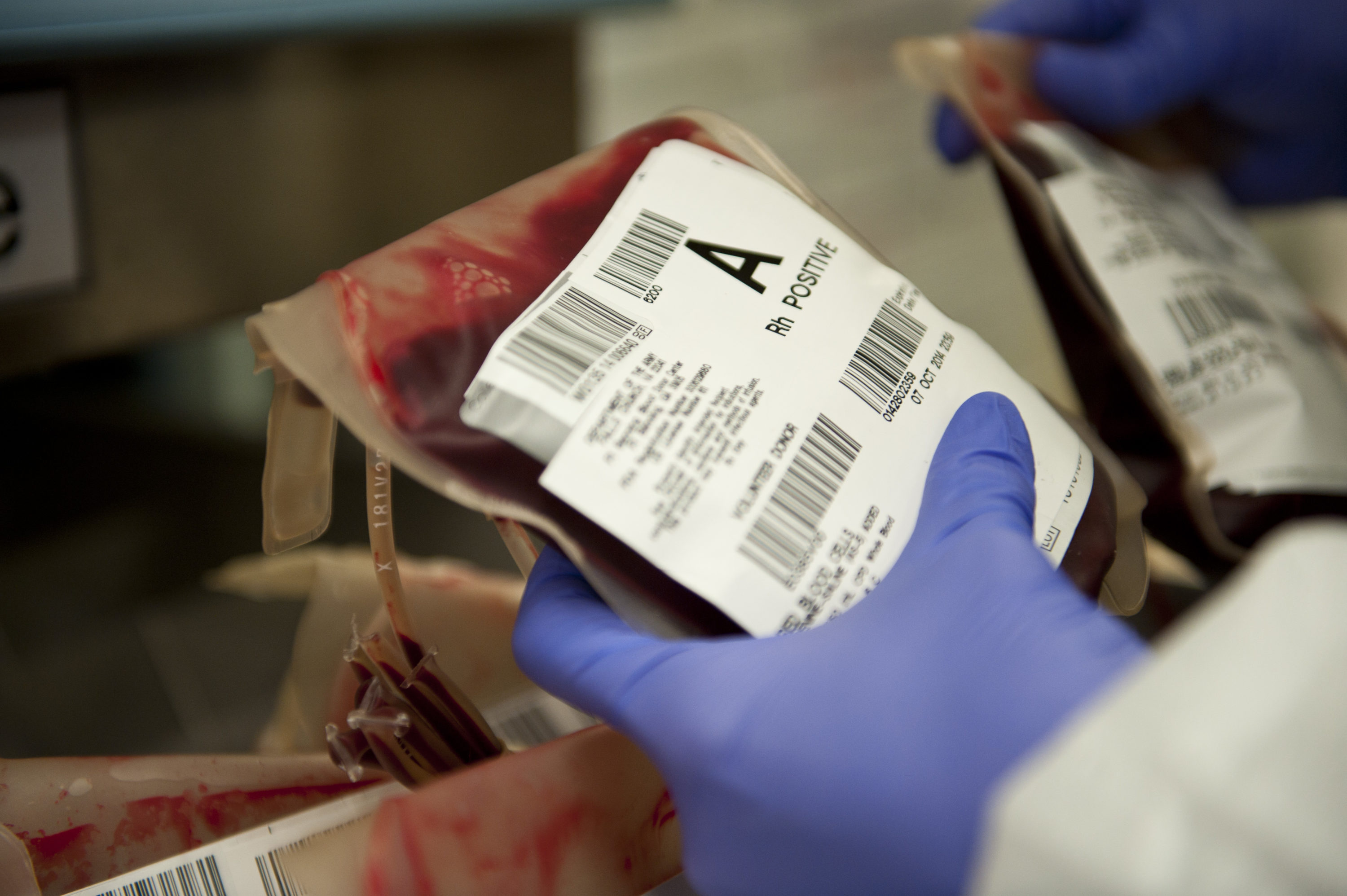
The trial, which began in 2017 and will continue until 2021, was to randomly assign 3,500 hospitalized patients at several dozen institutions throughout the U.S. and Canada who had suffered acute heart attacks and significant anemia one of two different treatments. A “liberal” strategy would give patients a transfusion at a higher red blood cell count level, while a “restrictive” strategy would give patients a transfusion when they reached a significantly lower red blood cell count level. The researchers were then going to see how many subjects from each group died or had another heart attack within 30 days. The trial was funded by the National Institutes of Health.
Public Citizen’s Health Research Group sent a detailed letter on Aug. 1, 2017 to the Office for Human Research Protections (OHRP) and the Veterans Affairs’ Office of Research Oversight (ORO) expressing concern that the trial lacked adequate protections for its human subjects and violated basic ethical principles. The restrictive transfusion strategy could put patients’ health and lives at unacceptable risk, and the trial protocol failed to provide key information, including a description of standard blood transfusion practices for heart attack patients. In addition, the sample consent forms failed to adequately describe the purpose of the research and the risks associated.
Public Citizen also called upon the researchers to conduct surveys or observational studies of current blood transfusions practices for heart attack patients at the participating institutions; revise the trial protocol to include all prior evidence that compared the liberal and restrictive strategies and explain how the MINT trial will affect the care of the patients at the institutions with enrolled subjects; revise the consent forms so the purpose of the research was adequately described and the risks of being assigned to one of the two strategies; and resubmit the revised protocol for review.
In June 2018, the OHRP and VA’s ORO responded, saying they were changing the protocol and consent forms. The changes included revising the protocol to better describe current care for patients experiencing acute heart attacks; adding a requirement that would not let a subject enroll unless their physician believed that either transfusion strategy would constitute good care for the subject; and adding to the consent form more details about the trial and the possible risks.
One of the most troubling ethical lapses in the MINT trial previously had been the failure of the consent form to fully disclose to potential subjects the possible risks of using a restrictive blood transfusion strategy. We are pleased to see that that the OHRP and ORO required changes that correct this ethical lapse and that address many of our other concerns.Dr. Michael Carome, director of Public Citizen’s Health Research Group.